Story highlights
A 77-year-old Japanese woman with age-related macular degeneration received a treatment of her own cells
Though her eyesight hasn't improved, it has stabilized, researchers say
In Florida, three elderly women were blinded by a different experimental stem cell treatment
As we grow older, a common disease called macular degeneration can threaten our eyesight. An experimental stem cell treatment proved effective at halting this disease with no serious side effects up to a year later, a study published Wednesday in the New England Journal of Medicine found. It is the first treatment using personalized, genetically identical cells derived from the patient.
However, serious concerns about such research persist. Three women with macular degeneration were blinded in 2015 after undergoing a stem cell treatment at a clinic in Florida. The patients experienced a variety of complications and are now blind, according to a paper published Thursday in The New England Journal of Medicine.
The macula is the spot in the center of your eye’s retina. When that tissue begins to thin and break down, this is referred to as macular degeneration, a blurring of the sharp central vision necessary for driving, reading and other close-up work. Most people develop this disease as they age.
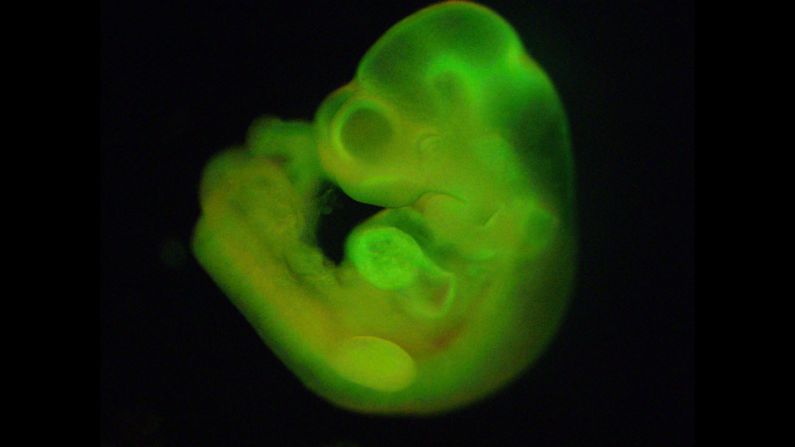
For the latest study, researchers led by Dr. Michiko Mandai of the laboratory for retinal regeneration at RIKEN Center for Developmental Biology in Japan tested an experimental stem cell treatment on a 77-year-old woman diagnosed with “wet,” or neovascular age-related, macular degeneration.
The “wet” form of the disease involves blood vessels positioned underneath the pigment epithelium (a layer of retinal cells) growing through the epithelium and harming the eye’s photoreceptor cells. In Japan, wet age-related macular degeneration is the most common form, but in Caucasian populations, only about 10% of people with age-related macular degeneration gets that form.
The “dry” form involves the macula breaking down without growth of blood vessels where they’re not supposed to be.
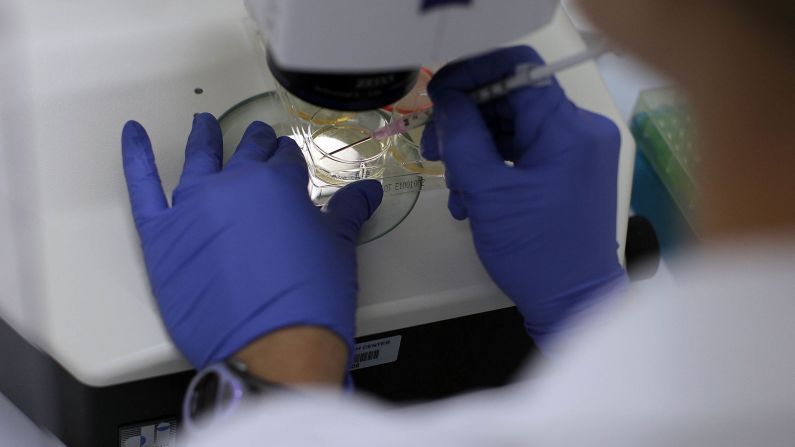
To stop the progress of wet macular degeneration, the researchers performed surgery to transplant a sheet of retinal pigment epithelial cells under the retina in one of the patient’s eye.
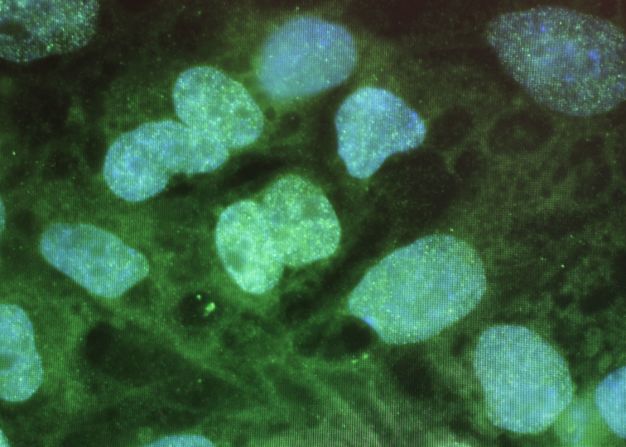
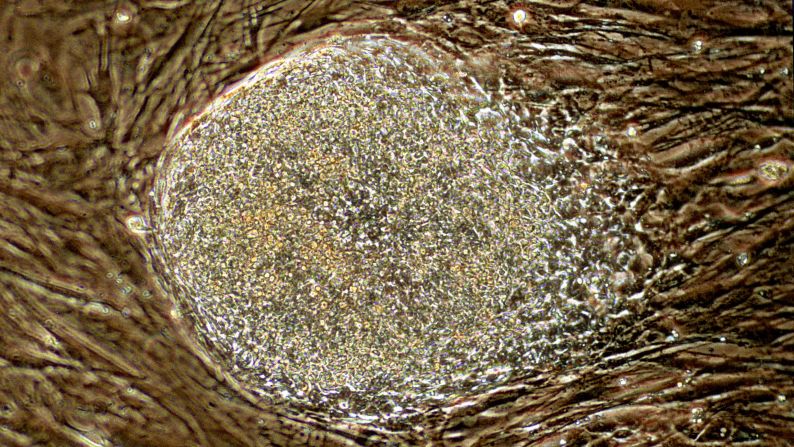
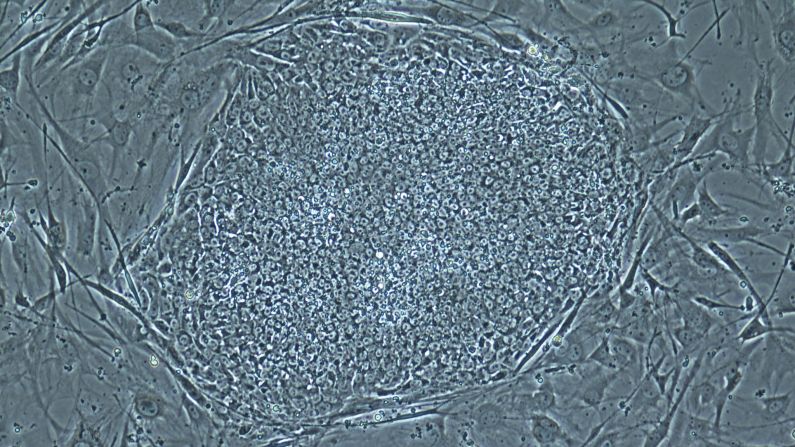
The transplanted cells had been derived from autologous induced pluripotent stem cells, which are reprogrammed cells. They were created using cells from the connective tissue of the woman’s skin.
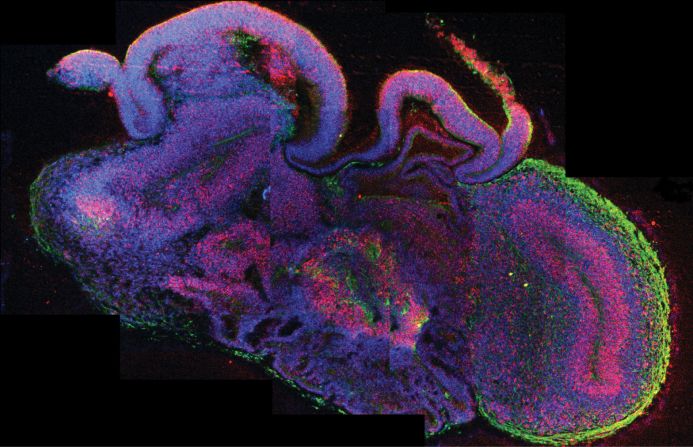
One year after surgery, the transplanted sheet remained intact, and there was no evidence of lasting adverse effects. Although the patient showed no evidence of improved eyesight, her vision had stabilized.
“This research serves multiple purposes,” wrote Peter Karagiannis, a science writer, in an email on behalf of Dr. Shinya Yamanaka, the Nobel Prize-winning co-author of the study and director of the Center for iPS Cell Research and Application at Kyoto University. From the patient’s perspective, the study shows that induced pluripotent stem cells can alleviate the problems associated with age-related macular degeneration.
“From a greater medical perspective, however, the bigger impact is that it shows iPS cells can be used as cell therapies,” the email said, adding that newly initiated stem cell research applications at the center include Parkinson’s disease and thrombocytopenia, a lack of platelets in the blood.
Another view of stem cell research
The Japanese study and the second study describing the blinding of three patients stand as “polar-opposite approaches to testing new therapies for age-related macular degeneration (AMD), which is a leading cause of blindness among elderly patients,” wrote Dr. George Q. Daley, dean of the faculty of medicine at Harvard Medical School, in an editorial published in the New England Journal of Medicine.
The American story, like the Japanese story, begins with patients slowly losing their sight as a result of macular degeneration – in this case, three women ages 72 to 88, two of whom had the “dry” form.
Each patient paid $5,000 for the procedure at an unnamed clinic in Florida, the authors noted. Some of the patients, including two of the three women described in the paper, learned of the so-called clinical trial on ClinicalTrials.gov, a registry database run by the US National Library of Medicine. However, the consent form and other written materials did not mention a trial.
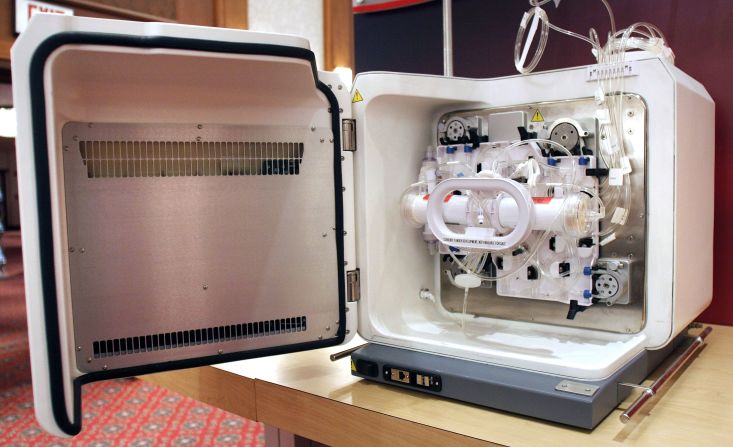
The procedure took less than an hour and began with a standard blood draw and the removal of fat cells from each patient’s abdomen. To obtain stem cells, the fat tissue was processed with enzymes, while platelet-dense plasma was isolated from the blood. The stem cells were mixed with the plasma and injected into both eyes.
Complications may have been caused by contamination during stem cell preparation, or the stem cells might have changed into myofibroblasts, a type of cell associated with scarring, after injection, the authors wrote.
Before the surgery, the women’s vision ranged from 20/30 to 20/200. After treatment and complications, the patients were referred in June 2015 to two university-based ophthalmology practices, including the University of Miami, where lead author Dr. Ajay E. Kuriyan was practicing.
“Many stem-cell clinics are treating patients with little oversight and with no proof of efficacy,” Kuriyan and his co-authors wrote in the paper, acknowledging that it is difficult for patients to know whether a stem cell therapy – or a clinical trial – is legitimate.
One red flag is that the patients were required to pay for their procedure; another is that both eyes were treated at once, the authors said. Legitimate clinical trials do not require payment, and for any experimental treatment of the eyes, a good doctor would observe how one eye responds before attempting the second eye.
Another problem for unsavvy patients: Listings on ClinicalTrials.gov are not fully scrutinized for scientific soundness, noted the authors.
Today, the clinic is no longer performing these eye injections, the authors said, but it is still seeing patients. In October 2015, months after the procedures had been performed, the Food and Drug Administration released more specific guidelines for stem cell treatments.
Writing on behalf of the FDA in an editorial alongside the paper, Drs. Peter W. Marks, Celia M. Witten and Robert M. Califf say there’s an absence of compelling evidence, yet some practitioners argue that stem cells have a unique capacity to restore health because of their ability to differentiate into whatever cell is necessary for repairing a defect. Another argument is that clinical trials are too complex for all except large industrial sponsors.
“Without a commitment to the principles of adequate evidence generation that have led to so much medical progress, we may never see stem-cell therapy reach its full potential,” Marks, Witten and Califf wrote in the New England Journal of Medicine.
The FDA has not approved any stem cell-based products for use, other than blood-forming stem cells for certain blood cancers, some inherited disorders and other specified indications. The agency recommends that consumers who are considering undergoing a stem cell treatment make sure it has been approved or is being studied in a clinical trial that the FDA has allowed.
An eye on stem cells
Despite the shadow cast by some stem cell experiments, the Japanese study earned praise from the scientific community.
Michael P. Yaffe, vice president of scientific programs at the New York Stem Cell Foundation Research Institute, said the RIKEN study was “incredibly thorough, careful and well-documented.”
“Many experts in the field of regenerative medicine believe that the treatment of macular degeneration and other retinal diseases will be among the first areas of success in the use of stem cell-derived tissues,” said Yaffe, whose foundation was not involved in the RIKEN study.
Yaffe said this optimism stems from preliminary studies using retinal cells derived from stem cells in animals. Scientists are also hopeful because the procedures to generate pure cells of the correct type and surgical techniques necessary for transplantation have already been developed.
“A number of research groups are moving toward developing stem cell-based treatments for age-related macular degeneration and other retinal diseases,” Yaffe said.
One, the London Project to Cure Blindness, has an ongoing clinical trial for a stem cell treatment. And an unrelated 2012 UCLA study showed that human embryonic stem cells restored the sight of several patients who had become nearly blind due to macular degeneration.
The National Eye Institute at the National Institutes of Health is planning a similar study using patient-specific pluripotent stem cells, according to Kapil Bharti, a Stadtman Investigator in the Unit on Ocular Stem Cell & Translational Research at the institute. After getting approval to conduct a phase I safety trial, the institute will treat 10 to 12 patients to check safety and tolerability of stem cell-based eye tissue transplants.
“Data from 10 to 12 patients is needed to show that the implanted cells are indeed safe,” he said, adding that the trial is likely to begin in 2018.
“While researchers have used embryonic stem cell derived cells to treat age-related macular degeneration, (the RIKEN study) is the first study that used induced pluripotent stem cells,” said Bharti, who was not involved in the research.
Both induced pluripotent stem cells and embryonic stem cells can be used to make other kinds of cells of the body, explained Bharti. However, induced pluripotent stem cells can be derived from adult skin or blood cells, rather than from embryos.
“Another big scientific advantage with induced pluripotent stem cells is that they can be made patient-specific (because it’s the patient’s own cells), reducing the chances of tissue rejection,” he said.
P. Michael Iuvone, a professor of ophthalmology and director of vision research at Emory University School of Medicine, also noted the importance of using the patient’s own stem cells.
Past studies have used embryonic stem cells to treat age-related macular degeneration, but there were problems related to rejection, when the body refuses to accept a transplant or graft, explained Iuvone, who was not involved in the latest study. In the new RIKEN study, the researchers took the patient’s own cells and converted them into retinal cells to avoid these complications.
“The results from the standpoint of the graft taking and surviving without any signs of any kind of toxicity or tumorigenicity are very positive,” Iuvone said. “But the weakness is, they only had one patient, and it’s very difficult to make any conclusions from one patient.”
He noted that the RIKEN researchers planned to work with more patients, but in 2014, the Japanese government passed a law that said regenerative medicine clinical trials could be performed only at medical institutions, not at research institutions such as RIKEN.
‘Major milestone’
Though the experiment was performed on a woman with wet age-related macular degeneration, it also might be useful for “dry” age-related macular degeneration, which is more common in the United States, according to Iuvone.
Currently, there are some effective treatments for age-related macular degeneration.
Join the conversation
“The standard of care in most cases is to give injections of drugs that inhibit the growth hormones that is called vascular epithelial growth factor, or VEGF,” Iuvone said. “For most people, it at least slows the progression and in some cases actually improves visual acuity.”
Laser treatments have also been used but are on the decrease because of side effects. “Given the fact that the VEGF treatments seem to be effective, I think that most clinicians have turned to that,” Iuvone said.
Bharti believes the RIKEN study is a major milestone in the field. “We and others are learning from the Japan study,” he said.
Susan L. Solomon, CEO of the New York Stem Cell Foundation Research Institute, agrees.
“This study represents a fundamental advance in regenerative medicine, in the use of stem cell-derived tissues and in the treatment of eye disease,” she said. However, additional work and many more studies are needed, she said, before a safe and efficacious stem cell-based treatment will be available “to the broad and growing population with retinal disease” – all of us, growing older.