Story highlights
14 patients at Massachusetts hospitals found to have a rare type of amnesia between 2012 and 2016
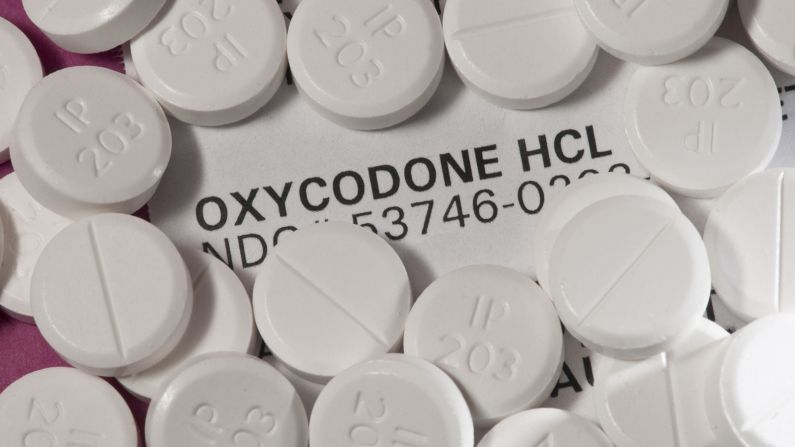
All but one patient tested positive for opioids or had a history of opioid abuse
More research is needed to understand the link between the two
What started with four patients with a puzzling form of amnesia turned into 14, and doctors are searching for others.
Dr. Jed Barash, a neurologist in the Boston area, noticed a patternbetween 2012 and 2015. Four patients, mysteriously stricken with a sudden amnesia, had the same rare finding on MRI: A pair of tiny structures deep in their brains, called the hippocampus, was completely knocked out on both sides.
The hippocampus is a seahorse-shaped structure that plays a role in memory and emotion. The patients could remember earlier things, but they couldn’t make new memories, a phenomenon called anterograde amnesia.
Also peculiar, three of the four patients tested positive for opioids. The fourth, who was not tested, was known to have a history of opioid abuse. The patients, ages 22 to 52, came to the hospital between October 2012 and November 2015.
“We couldn’t really address what was causing this,” said Dr. Alfred DeMaria Jr., the state epidemiologist for the Massachusetts Department of Public Health. DeMaria was contacted by Barash, who could not be reached for comment, to help investigate the cluster.
Doctors are trying to uncover whether these patients reveal an emerging syndrome related to substance use or whether it’s something else altogether.
Picking the brain for clues
The pattern seen on these patients’ MRIs was so rare that it had been described in only a handful of earliercase reports, including a couple of patients with cocaine abuse, one with carbon monoxide poisoning and one patient in France who had inhaled heroin, an opioid.
But now faced with the first known cluster of its kind, the Massachusetts Department of Health sent out a statewide alert in February, hoping to keep doctors on the lookout for additional cases.
They found 10 other patients who had been seen in eastern Massachusetts hospitals between 2012 and 2016, bringing the total to 14. All but one patient tested positive for opioids or had a history of opioid use. But none of these cases was fresh, making the search for a culprit all the more difficult.
“All we had was the medical records,” DeMaria said. “We couldn’t go back (in time).”
Though the MRI findings were described as “ischemic,” meaning there was a lack of blood flow to that part of the brain, it is unlikely that a stroke or lack of oxygen alone would cause such a specific and symmetrical injury to the hippocampus, said DeMaria.
“We’re really looking for a toxic effect,” he said.
DeMaria wondered whether the spate of new synthetic drugs and unknown contaminants on the illicit market might have something to do with it, but “we don’t even know if it’s related to drugs,” he said.
The story of Patient HM
The patients’ anterograde amnesia, along with their hippocampal injuries, reminded DeMaria of a famous lobotomy case from the 1950s: a patient known to most by his initials, HM, who lived most of his life without a hippocampus and suffered a similar, though more severe, anterograde amnesia.
Because the lack of a hippocampus may be similar to having an injured and nonfunctional one, some think that the Massachusetts cluster can reveal a lot about memory and the brain, as HM did.
“He’s one of the rare anonymous celebrities that you find in the history of science,” said Luke Dittrich, author of “Patient H.M.: A Story of Memory, Madness, and Family Secrets.”
When HM was 27 years old, in 1953, he had an experimental lobotomy to cure his severe epilepsy. The neurosurgeon who performed the lobotomy, which removed HM’s hippocampus and other surrounding structures, was Dittrich’s grandfather.
The surgery cured HM of his epilepsy, but it had a major unintended consequence: He couldn’t form new memories.
“He lived in 30-second increments,” Dittrich said. “The experiences in his life just washed off of him.”
But his personal tragedy was a boon to science, said Dittrich. Prior to HM, there was no consensus on which parts of the brain might be responsible for creating memories; it was widely thought that the brain worked as a whole to do so.
For over 50 years, memory scientists conducted tests on HM. When he died in 2008, his brain was sent to the University of California, San Diego. It was frozen, sliced into 2,401 sections and placed online for the general public to see.
“A lot of what we understand (about) how memory works has been built on top of the seminal studies that were done with HM,” Dittrich said.
Questions about the brain remain
Another curious aspect of HM’s amnesia, which may not be present in the Massachusetts patients, was that it “bleached away” the narrative of his memories before the surgery, said Dittrich. HM could remember facts about his childhood but not the stories to go along with them.
“We can all relate to memory loss,” Dittrich said. “But HM’s amnesia was even more alien to us than we typically imagine it to be.”
Barash’s descriptions of the Massachusetts patients did not include similar problems with prior memories, and some even showed improvement months later. The youngest patient, a 19-year-old and the only one without a history of opioid use, no longer had short-term memory loss five months later, though he also developed seizures.
Follow CNN Health on Facebook and Twitter
Still, Dittrich wonders what their similarities and differences might unearth about the human brain: why some recovered and some didn’t, whether some have issues with episodic memories in the past and what other cognitive effects their injuries might reveal.
“It’s a terrible tragedy,” Dittrich said, adding that the Massachusetts patients could nevertheless be “extremely valuable … to memory researchers.”
DeMaria said more research is needed to understand what happened and whether the link to opioids is more than coincidence. He also hopes doctors in other states keep an eye out for other cases that might be missed. For patients who test positive for opioids, doctors may easily mistake the signs of anterograde amnesia for general intoxication.
“Maybe nobody was looking for this,” DeMaria said. “Maybe this isn’t new. Maybe it was happening all along.”